Not Just Ozone Therapy, 8 Tips How To Manage Diabetes
Here are tips about how to manage diabetes with simple step. As a person who suffer diabetes, ozone therapy sounds familiar as alternative to maintain the blood sugar / glucose level. However, there are many things to consider when you are trying to improve your quality of life as your insulin is not in normal state anymore.
Diabetes is a chronic condition that occurs when your body cannot produce enough insulin, a hormone that regulates blood sugar, or when your body cannot effectively use the insulin it produces. This results in elevated levels of glucose in the blood, which over time can lead to serious damage to many of the body’s systems, including the heart and blood vessels.
Diabetes & Health Complications
When diabetes isn’t managed effectively, it can lead to a number of serious health complications, some of which can be life-threatening. These include:
Heart Disease and Stroke
Over time, high blood glucose from diabetes can damage your blood vessels and the nerves that control your heart. The longer you have diabetes, the higher the chances that you will develop heart disease. In adults with diabetes, the most common causes of death are heart disease and stroke.
Kidney Disease (Nephropathy)
Diabetes can damage the kidneys, which filter out waste products from your blood. This damage can lead to kidney failure or irreversible end-stage kidney disease, which may require dialysis or a kidney transplant.
Eye Damage (Retinopathy)
Diabetes can damage the blood vessels of the retina, potentially leading to blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma. Continuously, it will affect the vision of the sufferer-lowering the quality of life.

Nerve Damage (Neuropathy)
Excess sugar can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward. Poorly controlled blood sugar could cause you to eventually lose all sense of feeling in the affected limbs.
Specifically regarding heart failure, diabetes accelerates atherosclerosis, or the hardening of the arteries, causing coronary artery disease, heart attacks, and increasing the risk of heart failure. High blood sugars cause inflammation and oxidative stress, leading to changes in the heart’s structure and function, including stiffening of the heart muscle, increased thickness of the heart wall, and impaired relaxation of the heart. This can lead to both systolic and diastolic heart failure.
In addition, diabetes is often associated with other conditions that increase the risk of heart disease, such as high blood pressure and obesity. People with diabetes also tend to have unfavorable cholesterol levels, with higher levels of LDL (“bad”) cholesterol and triglycerides and lower levels of HDL (“good”) cholesterol, all of which increase the risk of heart disease.
In conclusion, managing blood sugar levels, maintaining a healthy lifestyle, and regularly monitoring for complications are essential for people with diabetes. This involves regular exercise, a healthy diet, controlling blood pressure and cholesterol levels, and avoiding smoking. Regular check-ups and screening for potential complications can also help to reduce the risk of severe complications.
How to Manage Diabetes Easily
Managing blood sugar levels often involves significant lifestyle changes. Here are several strategies that can help:
1. Healthy Eating: A balanced diet is crucial. Focus on whole foods and avoid highly processed items. Opt for lean proteins, whole grains, fruits, vegetables, and healthy fats. Try to limit consumption of sugary drinks and high-sugar foods. It’s also beneficial to eat regular meals to prevent blood sugar spikes and crashes.
2. Physical Activity: Regular exercise helps lower blood sugar levels and boost your body’s sensitivity to insulin. Strive for at least 30 minutes of moderate exercise, such as walking or cycling, most days of the week. Incorporate both cardio and strength training exercises into your routine for the best results.
3. Maintain a Healthy Weight: If you’re overweight, losing even a small amount of weight can have a big impact on your blood sugar levels. A healthcare provider can help you set realistic weight loss goals.
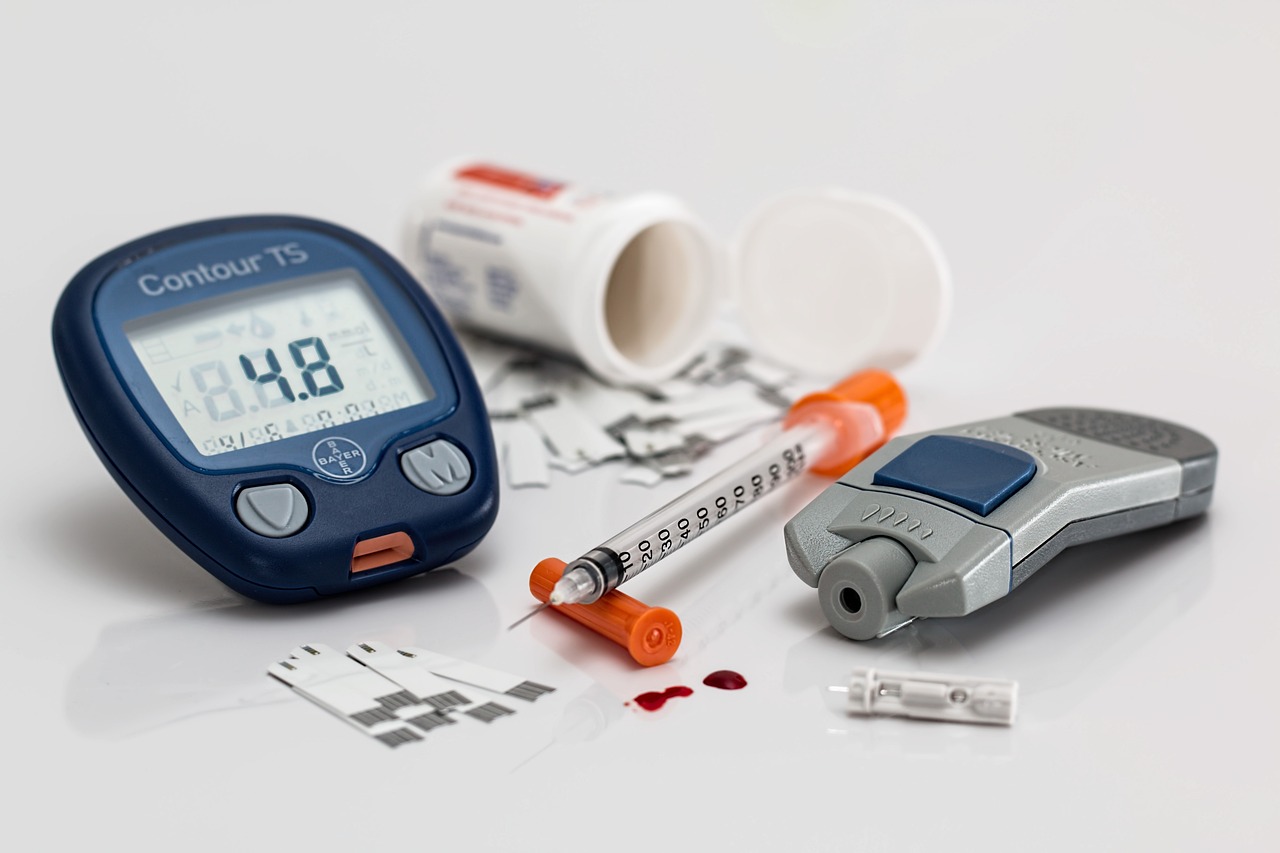
4. Regular Monitoring: Monitor your blood sugar levels regularly to ensure they’re within your target range. This can help you understand how different foods, activities, and stress affect your blood sugar levels.
5. Limit Alcohol: Alcohol can affect blood sugar levels, so drink in moderation. It’s also important to eat something when drinking to prevent low blood sugar. Alcohol can have complex effects on your blood sugar levels, and drinking can make it more difficult to manage diabetes. Here’s how:
- Hypoglycemia. If you’re using insulin or certain other diabetes medications that stimulate insulin production, drinking alcohol can increase the risk of hypoglycemia (low blood sugar). This is because the liver is responsible for removing toxins like alcohol from the body, but it’s also the organ that helps regulate blood sugar by releasing stored glucose. When the liver is busy metabolizing alcohol, it’s less efficient at regulating blood sugar, which can cause a drop in blood sugar levels.
- Hyperglycemia. On the other hand, many alcoholic drinks are high in sugar and calories, which can lead to high blood sugar levels or hyperglycemia. Beer and sweet wines, as well as cocktails mixed with soda and juice, can especially cause your blood sugar to spike.
- Weight Gain. Alcoholic beverages can be high in calories and may lead to weight gain over time, which can make blood sugar harder to control.
- Medication Interactions: Alcohol can interfere with the effectiveness of some diabetes medications and can increase their side effects.
- Impaired Judgment : Drinking alcohol can impair your judgment or lessen your resolve to manage your diabetes well, such as sticking to your eating plan or checking your blood glucose before going to bed.

In general, if you choose to drink alcohol, do so in moderation and always with a meal. Moderation generally means up to one drink a day for women and up to two drinks a day for men. However, guidelines may be different depending on your age, overall health, and the type of diabetes medications you take, so it’s best to talk to your doctor about what’s appropriate for you.
Also, it’s a good idea to check your blood sugar before you go to sleep after drinking alcohol, to make sure it’s at a safe level, because alcohol can lower blood sugar levels for up to 24 hours after drinking.
6. Quit Smoking: Smoking increases the risk of diabetes complications, including heart disease. If you smoke, ask your doctor about strategies to help you quit.Smoking can have a detrimental impact on your blood sugar levels and overall diabetes management. Here’s how:
- Insulin Resistance: Nicotine, the addictive component in cigarettes, can make your body more resistant to insulin. This can lead to higher blood sugar levels because your body is not able to use insulin effectively to move glucose into cells for energy.
- Inflammation and Oxidative Stress: Smoking leads to inflammation and oxidative stress in the body. These can also increase insulin resistance and affect how well your body can regulate blood sugar.
- Weight Management: Smoking is often associated with appetite suppression and weight loss, but it may also increase abdominal fat, which is linked to insulin resistance. After quitting smoking, some people may initially gain weight. However, in the long run, quitting smoking can make it easier to exercise and maintain a healthy weight, which is beneficial for blood sugar control.
- Complications: People with diabetes who smoke are at higher risk for heart disease, kidney disease, and nerve damage—all potential complications of diabetes. These conditions can, in turn, make it harder to manage your diabetes.
- Poor Healing: Smoking affects the circulation by narrowing the blood vessels, which can slow down wound healing—a common issue for people with diabetes. Poor wound healing can increase the risk of infections, which can cause blood sugar levels to rise.
Given these risks, quitting smoking is one of the most important steps you can take for your overall health and for better diabetes management.
7. Manage Stress: Stress can affect your blood sugar levels. Techniques such as yoga, meditation, or other relaxation techniques can help manage your stress levels.When you’re stressed, your body goes into “fight or flight” mode, which is its way of responding to perceived threats. This causes various physiological changes, including the release of certain hormones such as adrenaline (also called epinephrine), cortisol, glucagon, and growth hormone.
These hormones trigger the liver to produce more glucose, the body’s main source of energy, to provide a quick energy boost for the body to cope with the stressor. For people without diabetes, the body responds to this rise in blood sugar by producing more insulin, which helps cells take in the extra glucose for energy and brings blood sugar levels back to normal.
However, if you have diabetes, your body either doesn’t produce enough insulin (Type 1 diabetes) or can’t use insulin effectively (Type 2 diabetes). This means that during times of stress, your body may not be able to efficiently use or absorb the extra glucose that’s released, leading to higher blood sugar levels.
Chronic stress can also make it harder to manage diabetes. You may forget to check your blood sugar levels, eat healthy, exercise, or even take your medications, all of which can lead to poor blood sugar control.
If you’re experiencing frequent or severe stress, it’s important to talk to your healthcare provider. They can suggest strategies to help you manage stress, such as relaxation exercises, physical activity, and counselling. It may also be necessary to adjust your diabetes treatment plan to better manage your blood sugar levels during times of stress.
8. Regular Check-ups: Regular medical check-ups are crucial to ensure your diabetes is under control and to monitor for any potential complications.
These lifestyle changes can greatly help manage blood sugar levels, but they’re not a substitute for medical treatment. If you have been prescribed medication, it’s important to take it as directed by your healthcare provider. Always consult with your healthcare provider before starting any new diet or exercise regimen.